ERCP
Original Article Korean J Pancreas Biliary Tract 2019; 24(1): 21-30. Published online: January 31, 2019 한국의 내시경적 역행성 담췌관 조영술에 대한 전국적인 실태 조사Practice of Endoscopic Retrograde Cholangiopancreatography in Korea: Results from a National Survey
Dong-Won Ahn1, Joung-Ho Han2, Hong Ja Kim3, Hyung-Keun Kim4, Byoung Kwan Son5, Sun Young Yi6, Ju Sang Park7, Eaum Seok Lee8, Hyunsoo Kim9, Kwang Bum Cho10, Ho Gak Kim11, Seon Mee Park2
1Department Internal Medicine, Seoul National University Boramae Medical Center, Seoul, Korea 2Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea 3Department of Internal Medicine, Dankook University College of Medicine, Cheonan, Korea 4Department of Internal Medicine, Uijeongbu St. Mary's Hospital, The Catholic University College of Medicine, Uijeongbu, Korea 5Department of Internal Medicine, Eulji University College of Medicine, Seoul, Korea 6Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea 7Division of Gastroenterology, Department of Internal Medicine, Bundang Jesaeng General Hospital, Seongnam, Korea 8Department of Internal Medicine, Chnungnam National University College of Medicine, Daejeon, Korea 9Department of Internal Medicine, Daegu Fatima Hospital, Daegu, Korea 10Department of Internal Medicine, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea 11Department of Internal Medicine, Daegu Catholic University School of Medicine, Daegu, Korea Corresponding author : Seon Mee Park Department of Internal Medicine, Chungbuk National University Hospital, Chungbuk National University College of Medicine, 1 Chungdae-ro, Seowon-gu, Cheongju 28644, Korea Tel. +82-43-269-6019 Fax. +82-43-273-3252 E-mail; smpark@chungbuk.ac.kr
Copyright © 2019 by The Korean Journal of Pancreas and Biliary Tract This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original work is properly cited. 요약결과ERCP 의사 157명 중에서 129명이 설문에 응답하여 82.2%의 회수율을 보였다. 한국에서 ERCP 시행률은 지속적으로 증가하였다. 약 반수의 의사는 1인당 ERCP 양이 연간 200예 이상으로 시술량이 많은 ERCP 의사에 속하였다. 대부분의 ERCP 의사들은 1단계의 ERCP 시술을 시행하였으나 담췌관 내압 측정, 담관-췌관경 및 췌장 시술은 많은 양의 시술을 하는 병원에서만 시행하였다. 대부분의 ERCP 의사들은 90% 이상의 성공률을 보였으나, 예비 괄약근 절개율이 약 25%로 표준질지표보다 높았다. 12명의 ERCP 의사들이 최근 1년간 ERCP 후 환자가 사망하는 합병증을 경험하였다. 또한 ERCP 수련과 시술량이 낮거나 중등도인 병원의 방사선 차폐는 표준 질지표에 도달하지 못하였다.
Keywords: 췌담도 조영술, 내시경적 역행성, 설문 조사 및 설문지, 질지표, 대한민국 AbstractBackground/AimsThe aim of this study is to describe the outcome of the national survey and to determine the endoscopic retrograde cholangiopancreatography (ERCP) quality in Korea by comparing with the quality indicators.
MethodsWe used the database of Health Insurance Review & Assessment Service and then performed anonymous national survey.
ResultsCompleted questionnaires were returned by 129 of 157 ERCP endoscopists. In Korea, annual ERCP rates have been consistently increased over years. Individual ERCP volume was high (>200 per year) in about half of ERCP endoscopists. Most ERCP endoscopists performed all of level I procedures. However, manometry, cholangiopancreatoscopy, and pancreatic procedures were performed mostly in institutions with high hospital volume. The rate of overall success was more than 90% in most ERCP endoscopists. However, the rate of precut sphincterotomy was high in more than a fourth of ERCP endoscopists. Twelve ERCP endoscopists experienced post-ERCP mortality within recent 1 year. ERCP training and radiation protection during ERCP did not meet the standard of quality indicators especially in institutions with low or moderate hospital volume.
ConclusionsTechnical issues during ERCP procedures in Korea fulfill the standard of quality indicators. However, a great effort is needed to improve issues about ERCP training and radiation protection.
Keywords: Cholangiopancreatography, Endoscopic retrograde, Surveys and questionnaires, Quality indicators, Republic of Korea INTRODUCTIONWith the advent of magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasonography (EUS), diagnostic endoscopic retrograde cholangiopancreatography (ERCP) has been replaced by these non-invasive imaging tests [1]. However, ERCP is still an important tool in the nonsurgical management of various pancreatobiliary diseases [2]. ERCP is one of the most advanced and technically demanding endoscopic procedures with a considerable risk of complications [3]. In an effort to raise the quality of ERCP procedures, several quality indicators for ERCP have been proposed [3-6] and national survey of ERCP practice based on the quality indicators have been performed worldwide [1,2,7-11].
In South Korea, more than 50,000 ERCPs are performed each year and the annual ERCP rates are consistently increasing. To date, however, there are limited data about the ERCP practice in Korea because of lack of nationwide studies about this issue [12]. Therefore, the Korean Pancreatobiliary Association (KPBA) conducted a national survey to determine the ERCP practices and quality outcomes in Korea. The aim of this study is to describe the outcome of the national survey and to determine the ERCP quality by comparing with the quality indicators that have been proposed. We conducted national surveys about ERCP after analyzing national data obtained from Health Insurance Review & Assessment Service (HIRA) to give meaning to them. This survey provided the level of ERCP quality in Korea and quality indicators, which did not fulfill the quality requirements.
METHODS1. Investigation of annual ERCP ratesTo investigate total number of ERCP in Korea, we used the database of HIRA. In Korea, all surgical and endoscopic procedures including ERCP are registered to the database of HIRA. With the database, we investigated the total number of ERCP from 2010 to 2014. According to the database of HIRA, hospital type is categorized into four groups based on the number of occupied beds university hospital, general hospital, hospital, and clinic. So, the number of ERCP was investigated according to the four hospital types separately. To determine the ERCP availability in Korea and to compare it to those in other countries, the 1-year ERCP rate was used a main index to represent the status of ERCP availability [9]. The ERCP rates of other countries were retrieved or calculated through published data resources [10,11,13-18].
2. Conduct of the surveyAn online survey was conducted from July 2015 to September 2015. According to the registry of the KPBA, there were a total of 157 ERCP endoscopists worked in 2015. E-mail with direct access to web link survey was sent to them for six times with an interval of 2 weeks. The online survey was performed with a predesigned standard structured questionnaire. A pilot version was sent to a group of 15 ERCP endoscopists including members of the KPBA who were participated to prepare the questionnaire to confirm the clarity and suitability of each question. We implemented minor revisions based on review of the pilot version before its widespread administration. The final questionnaire consisted of a total 40 questions and the contents of the questionnaire were classified into five categories: 1) volume, indication, and preparations of ERCP; 2) ERCP procedures; 3) ERCP training; 4) ERCP complications, and 5) radiation protection during ERCP. A returned questionnaire was considered valid if all of the required information was provided.
3. Categorization of ERCP volumesWe classified annual ERCP volumes (both in each hospital and each ERCP endoscopist) into three categories: high volume (HV) (>200 cases/year), moderate volume (MV) (50-200 cases/year), and low volume (LV) (<50 cases/year). The rationale of this classification was based on previous studies reported relationship between ERCP volume and complications [14,19,20], previous guidelines about an appropriate number of ERCP for competency [21-23], and a previous survey in other countries [1].
4. Statistical analysisCategorical data were presented as proportions and continuous variables were presented as mean±standard deviation. To measure differences in each of these categories across all three volume groups, we used Pearson’s x2 test for independence and standard x2 test for pairwise comparisons. We considered a 2-tailed α error of <0.05 to represent statistical significance. All statistical analyses were performed by using SPSS version 13.0 for Windows (SPSS Inc, Chicago, IL, USA).
RESULTS1. Annual ERCP rates in KoreaAccording to the data from HIRA, the number of ERCP has been consistently increased over years (Fig. 1). A total of 40,162 and 47,983 ERCP were performed in 2010 and 2014, respectively. More than 80% of ERCP were therapeutic ERCP in each year. Investigation of the number of ERCP among four hospital types showed that most ERCP (more than 99%) were performed in university hospital or general hospital in Korea (Fig. 2). When we calculated the annual ERCP rate in 2010 in Korea, the annual ERCP rate was 82.6 per 100,000 inhabitants (4.86 million as the total population). The comparison between Korea and other countries is shown in Fig. 3 [11].
2. Response to the surveyOf the 157 endoscopists questioned, 129 (82.2%) responded and completed questionnaires. There were 71 endoscopists in university hospitals (56%), 54 in general hospitals (42%), and three in hospitals (2%). Experience of ERCP was more than 10 years in 52 (41%), 5 to 10 years in 38 (30%), 1 to 5 years in 33 (26%), and less than 1 year in four (3%).
3. Volume and preparations of ERCPAnnual hospital ERCP volume was HV in 92 (72%), MV in 27 (21%), and LV in nine (7%). And annual individual ERCP volume was HV in 62 (49%), MV in 53 (42%), and LV in 12 (9%). Only 31 respondents (24%) performed ERCP in outpatients. The rate of diagnostic ERCP was less than 5% in more than 80% of respondents.
An informed consent before ERCP was achieved by ERCP endoscopist only in 21 respondents (16%), and more than 80% of respondents reported that an informed consent was achieved by trainee or medical resident. Prophylactic antibiotic administration was performed during all therapeutic ERCP in 84 (63%).
4. Indications of ERCPWe classified the indications of ERCP into grades of difficulty ranging from I to III according to criteria established by Ang et al. [5] More than 90% of respondents across all groups (LV, MV, and HV) performed most of level I procedures except cytology. For level II and III procedures, large common bile duct (CBD) stone (>10 mm) removal, drainage for hilar tumors or benign intrahepatic strictures, precut sphincterotomy, and lithotripsy was performed by more than 85% of respondents. However, other level II and III procedures such as minor papilla cannulation (58.9%), manometry (11.6%), cholangiopancreatoscopy (45.7%), therapeutic ERCP in Billroth II anastomosis (78.3%), pancreatic procedure such as pseudocyst drainage (60.5%), and intrahepatic duct (IHD) stone removal (61.2%) was performed by less than two-thirds of respondents. Table 1 summarizes the proportions of respondents who would perform Level I, II, or III procedures according to individual volume. Respondents with moderate or high individual volume were more likely to perform level II or III procedures. Considering that institutions with high hospital volume are more likely to possess the equipment necessary for manometry, cholangiopancreatoscopy, or pancreatic procedure (such as pseudocyst drainage), we investigated the relationship between these procedures and hospital volume. Respondents in high hospital volume were more likely to perform manometry, cholangiopancreatoscopy, and pancreatic procedure (such as pseudocyst drainage) than those in low or moderate hospital volume (Table 2).
5. ERCP proceduresAs sedative agents during ERCP, 45 respondents (35%) used only midazolam, and 80 respondents (53%) used propofol (with or without midazolam). Fourteen respondents (11%) reported that propofol was used with participation of anesthesiologist for patient monitoring during ERCP.
Time for attempt at bile duct cannulation was within 30 minutes in most respondents (except one), and all respondents attempted bile duct cannulation less than 20 times before termination. However, 34 respondents (26%) performed precut endoscopic sphincterotomy (EST) in more than 10% of case for bile duct cannulation.
Most respondents (except two) performed successful bile duct cannulation through native papilla more than 85%, and in 63 (49%) of them, the rate was more than 95%. The overall therapeutic procedures including CBD stone removal and biliary drainage was more than 90% in most respondents.
6. ERCP trainingDuring the training period of trainee, the number of ERCP training was less than 150 cases in 87 respondents (67%), and less than 30 cases in 45 respondents (35%). The number of therapeutic ERCP training was less than 50 cases in 86 (67%).
7. ERCP complicationsWe investigated the number of severe complications such as cholangitis, pancreatitis and perforation in each endoscopist within one year before the response to the questionnaire. The definitions of severe ERCP complications are same as those in previous report [24]. A total of 79 respondents (61%) experienced the severe ERCP complications within one year. The number of severe complications within one year was less than five cases in 69 respondents, and five to 10 cases in seven respondents. One respondent experienced more than 10 cases of severe complications within 1 year. Twelve respondents (9.3%) reported that they experienced complication-related mortality within recent 1 year. Among them, six respondents experienced medical disputes including lawsuit.
8. Radiation protection during ERCPWe investigated the frequency of actual use of the essential protective equipment: lead apron, thyroid shields, lead glasses, lead fabrics, and lead-containing mobile glass. Table 3 summarizes the frequency of actual use of the protective equipment. More than 90% of respondents used lead aprons and thyroid shields almost always. However, the frequency of actual use of lead glasses, lead fabrics, or lead-containing mobile glass was very low. More than half of respondents used lead glasses, lead fabrics, or lead-containing mobile glass in less than 50% of ERCP cases. When we analyzed the relationship between the actual use of protective equipment and hospital volume, the rate of actual use of lead glasses, lead fabrics, or lead-containing mobile glass was significantly lower in respondents in LV or MV hospital than HV hospital (36.1% vs. 73.6%). The location of radiation source was over-couch in 97 respondents (76%) and under-couch in 31 respondents (24%). Among 97 respondents with over-couch radiation source, only 50 respondents (52%) reported having lead shields such as lead fabrics or lead-containing mobile glass.
The frequency of actual putting on radiation dosimeters is also summarized in Table 3. About 50% of both ERCP endoscopists and assistants did not put on the radiation dosimeters during ERCP. The location of the radiation dosimeters was chest inside lead apron in 83 (85%), chest outside lead apron in eight (8%), and neck inside thyroid shield in five (5%), respectively.
When we investigate the results of regular radiation monitoring during ERCP, seven respondents (6%) reported that they have experienced the excess of upper limit of radiation proposed from the International Commission on Radiological Protection Recommendation (ICRP) [25] that a person can safely be exposed to in a year (20 millisivert). Furthermore, 53 respondents (43%) reported that they have not measured radiation exposure on a periodic basis.
With regard to the 2009 ERCP-related radiation damage prevention recommendations of the KPBA, 96 (75%) respondents have attended lectures or read documents on the subject. Among these 96 respondents, 72 (75%) reported a changed awareness about radiation protection and an additional effort to improve the radiation protection such as purchase of additional protective equipment, use of protective equipment all the times, or initiation of radiation monitoring.
DISCUSSIONThis national survey is the first comprehensive survey on the ERCP practice in Korea. According to the database of HIRA, the number of ERCP in Korea has been consistently increased reaching more than 50,000 since 2016. The annual ERCP rate in Korea was 82.6 per 100,000 inhabitants in 2010, which is not inferior to those in other developed countries.
Although ERCP volume is not inferior to those in other developed countries, it would be problematic that most ERCP services in Korea are provided by university hospital or general hospital. In other developed countries, in contrast, ERCP service provided by community health providers covers a substantial proportion of population, with the success rate and adverse event rate of routine ERCP being comparable or slightly inferior to those at academic medical centers [8,26-28]. Because the database of HIRA shows that ERCP services provided by hospital or clinic (small community health providers) covers a minimal proportion (less than 1%), we can expect that individual ERCP volume in these community health providers would be very low in Korea. Although the association between the ERCP volume and the quality and outcome of ERCP has not been conclusive [11], many studies show positive relationships between the ERCP volume and the outcome of ERCP. A recent large prospective, multicenter study from Austria showed greater technical success and fewer complications by endoscopists performing more than 50 ERCPs per year [14]. Studies in Sweden [10] and Italy [29] showed better outcomes in institutions doing more than 200 ERCPs per year. In North America, Freeman et al. [19] showed that ERCP endoscopists doing more than 50 sphincterotomies per year were more successful and had fewer complications, especially less severe ones. Based on the results of these previous studies, some experts argue that anyone performing fewer than 50 ERCP per year should consider carefully their reasons for continuing and those who wish to continue should justify their decision by collecting performance data prospectively [30]. Considering very low ERCP volume in the small community health providers in Korea, a great effort should be made to improve quality of ERCP practice.
In the results about ERCP indications in our survey, most ERCP endoscopists across all groups (LV, MV, and HV) performed all of level I procedures. And most ERCP endoscopists also performed large CBD stone (>10 mm) removal, drainage for hilar tumors or benign intrahepatic strictures, precut sphincterotomy, and lithotripsy. However, ERCP endoscopists with individual LV were less likely to perform most of level II or III procedures such as minor papilla cannulation, drainage for hilar tumors or benign intrahepatic strictures, precut sphincterotomy, therapeutic ERCP in Billroth-II anastomosis, lithotripsy, and IHD stone removal. And ERCP endoscopists in LV or MV hospital were less likely to perform manometry, choangiopancreatoscopy, or pancreatic procedure. These results are similar to those from a previous survey in other countries [1].
In this survey, most respondents showed more than 85% of successful bile duct cannulation through native papilla and more than 90% of success in CBD stone removal and biliary drainage. Therefore, most respondents reached more than 85% of successful therapeutic procedures. These results fulfill the standard of quality indicators that have been proposed [3-6]. In our survey, time for attempt at bile duct cannulation was within 30 minutes in most respondents, and all respondents attempted bile duct cannulation less than 20 times before termination. These results are somewhat different from those from a previous survey in other country, in which not a few HV endosopists persisted more than 30 minutes and with greater attempts at bile duct cannulation before terminating the procedure [1]. Guidelines from the American Society for Gastrointestinal Endoscopy (ASGE) suggests that most experienced endoscopists do not rely on precut EST methods in more than 10 to 15% of cases and these precut methods should not be used as an alternative to proper cannulation techniques [3]. In our survey, however, more than a fourth of ERCP endoscopists performed precut EST in more than 10% of case for bile duct cannulation. According to the results in our survey, we can expect that not a few ERCP experts in Korea prefer early precut EST rather than persistent attempt of conventional cannulation in case of difficult bile duct cannulation.
To date, there is no international consensus regarding the minimum standards for ERCP training and accreditation [2]. The ASGE has suggested an 80% success rate in cannulation/basic treatment as a benchmark for competence [31]. And a study from Duke University reported that their fellows were only approaching 80% competence after performing 180 to 200 ERCPs [21]. In the UK, the Joint Advisory Group on Gastrointestinal Endoscopy has indicated that trainees should perform at least 180 ERCPs under supervision, and they cannot be considered competent in ERCP until they can cannulate the desired duct in over 90% of cases [12,32]. In the results about ERCP training of our survey, most ERCP endoscopists, during their periods of trainee, were insufficiently trained to perform ERCP. The number of ERCP training was less than 150 cases in two thirds of respondents, and a third of respondents reported that they have been trained to perform ERCP with less than 30 cases. In Korea, while the number of institutions in which ERCP can be performed is consistently increasing, the number of institutions in which sufficient ERCP training can be provided to trainees is not nationally sufficient yet. Furthermore, duration of ERCP training is too short for fellows to gain adequate experience of ERCP in real clinical practice in most institutions. Although the problem of large numbers of ERCP trainees performing relatively few ERCP procedures is not unique to Korea [2], an awareness of this problem should be increased and consideration to improve ERCP training should be made in future.
Protective equipment is essential to reduce radiation exposure during ERCP procedure [33]. The ASGE recommends that all health care providers wear lead aprons and have thyroid shields in place in order to practice ERCP, that those performing ERCP close to their patients should wear lead glasses as well, and that lead shields should be set up in front of those performing ERCP [34]. In the results about radiation protection in our survey, most endoscopists put on lead apron and thyroid shield actually during ERCP, however, the rate of actual use of lead glasses, lead fabrics, or lead-containing mobile glass was low especially in LV or MV hospitals. Half of respondents who reported to have overcouch radiation source reported that they did not have lead shields. Radiation dosimeter is a crucial tool in drawing attention to radiation hazards. However, in our survey, about half of respondents (both ERCP endoscopists and assistants) did not put on the radiation dosimeters during ERCP. Furthermore, more than 40% of respondents reported that they have not measured radiation exposure on a periodic basis. KPBA has already performed a national survey of radiation exposure protection and has reported the results of the survey in 2013 [33]. The results of this previous survey are similar to those of our survey. However, the rate of respondents who have attended lectures or read documents on the 2009 ERCP-related radiation damage prevention recommendations of the KPBA was increased in our survey compared to that in the previous survey (from 40% to 75%) [33]. And considerable proportions of these respondents reported a changed awareness about radiation protection and an additional effort to improve the radiation protection. Therefore, a persistent nationwide promotion of the recommendations by KPBA would help to improve practice of radiation protection.
There are limitations in our study. First, the questionnaire of this survey was retrospective and retrospective one which could not avoid recall bias. Second, because the survey relating the questions about severe ERCP complications relied on the estimation of each respondent, the incidence of severe complications could not be assessed both nationally and separately to each institution, which is an important issue in ERCP. While 12 ERCP endoscopists reported that they experienced post-ERCP mortality within recent 1 year, the exact frequency of mortality could not be assessed either. And, the relationship between the ERCP volume and the incidence of severe complications could not be analyzed. Third, this survey was questioned only to ERCP endoscopists registered to the registry of the KPBA rather than performed to ERCP endoscopists who work in hospital or clinic and were not registered to the KPBA registry. However, considering that most ERCP procedures (more than 99%) are performed in university hospital or general hospital in Korea, the findings of this survey would be representative of the status of ERCP practices in Korea.
In conclusion, annual ERCP rates in Korea have been consistently increased over recent years. Technical issues during ERCP procedures in Korea fulfill the standard of quality indicators. However, ERCP training and radiation protection during ERCP did not meet the standard of quality indicators especially in institutions with low and moderate hospital volume. A great effort is needed to improve issues about ERCP training and radiation protection.
REFERENCES1. Coté GA, Keswani RN, Jackson T, et al. Individual and practice differences among physicians who perform ERCP at varying frequency: a national survey. Gastrointest Endosc 2011;74:65-73 e12.
2. Williams EJ, Taylor S, Fairclough P, et al. Are we meeting the standards set for endoscopy? Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut 2007;56:821-829.
3. Baron TH, Petersen BT, Mergener K, et al. Quality indicators for endoscopic retrograde cholangiopancreatography. Am J Gastroenterol 2006;101:892-897.
4. Adler DG, Lieb JG 2nd, Cohen J, et al. Quality indicators for ERCP. Gastrointest Endosc 2015;81:54-66.
5. Ang TL, Cheng J, Khor JL, et al. Guideline on training and credentialing in endoscopic retrograde cholangiopancreatography. Singapore Med J 2011;52:654-657.
6. Springer J, Enns R, Romagnuolo J, Ponich T, Barkun AN, Armstrong D. Canadian credentialing guidelines for endoscopic retrograde cholangiopancreatography. Can J Gastroenterol 2008;22:547-551.
7. Cotton PB, Romagnuolo J, Faigel DO, Aliperti G, Deal SE. The ERCP quality network: a pilot study of benchmarking practice and performance. Am J Med Qual 2013;28:256-260.
8. Colton JB, Curran CC. Quality indicators, including complications, of ERCP in a community setting: a prospective study. Gastrointest Endosc 2009;70:457-467.
9. Liao Z, Hu LH, Xin L, Li ZS. ERCP service in China: results from a national survey. Gastrointest Endosc 2013;77:39-46 e1.
10. Enochsson L, Swahn F, Arnelo U, Nilsson M, Löhr M, Persson G. Nationwide, population-based data from 11,074 ERCP procedures from the Swedish Registry for Gallstone Surgery and ERCP. Gastrointest Endosc 2010;72:1175-1184 e1-e3.
11. Hu LH, Xin L, Liao Z, et al. ERCP development in the largest developing country: a national survey from China in 2013. Gastrointest Endosc 2016;84:659-666.
12. Kim J, Park ET, Son BK, et al. ERCP educational guidelines for fellows. Korean J Pancreas Biliary Tract 2017;22:1-13.
13. Bodger K, Bowering K, Sarkar S, Thompson E, Pearson MG. All-cause mortality after first ERCP in England: clinically guided analysis of hospital episode statistics with linkage to registry of death. Gastrointest Endosc 2011;74:825-833.
14. Kapral C, Duller C, Wewalka F, Kerstan E, Vogel W, Schreiber F. Case volume and outcome of endoscopic retrograde cholangiopancreatography: results of a nationwide Austrian benchmarking project. Endoscopy 2008;40:625-630.
15. Glomsaker T, Søreide K, Aabakken L, Søreide JA. A national audit of temporal trends in endoscopic retrograde cholangiopancreatography in Norway. Scand J Gastroenterol 2011;46:116-121.
16. Ekkelenkamp VE, de Man RA, Ter Borg F, et al. Prospective evaluation of ERCP performance: results of a nationwide quality registry. Endoscopy 2015;47:503-507.
17. Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012;143:1179-1187 e3.
18. Baudet JS, Borque P, Borja E, et al. Use of sedation in gastrointestinal endoscopy: a nationwide survey in Spain. Eur J Gastroenterol Hepatol 2009;21:882-888.
19. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med 1996;335:909-918.
20. Rabenstein T, Schneider HT, Nicklas M, et al. Impact of skill and experience of the endoscopist on the outcome of endoscopic sphincterotomy techniques. Gastrointest Endosc 1999;50:628-636.
21. Jowell PS, Baillie J, Branch MS, Affronti J, Browning CL, Bute BP. Quantitative assessment of procedural competence. A prospective study of training in endoscopic retrograde cholangiopancreatography. Ann Intern Med 1996;125:983-989.
22. Chutkan RK, Ahmad AS, Cohen J, et al. ERCP core curriculum. Gastrointest Endosc 2006;63:361-376.
23. Eisen GM, Dominitz JA, Faigel DO, et al. Guidelines for advanced endoscopic training. Gastrointest Endosc 2001;53:846-868.
24. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc 1991;37:383-393.
25. 1990 recommendations of the international commission on radiological protection. Ann ICRP 1991;21:1-201.
26. Dumonceau JM, Rigaux J, Kahaleh M, Gomez CM, Vandermeeren A, Devière J. Prophylaxis of post-ERCP pancreatitis: a practice survey. Gastrointest Endosc 2010;71:934-939.
27. Rabago L, Guerra I, Moran M, et al. Is outpatient ERCP suitable, feasible, and safe? The experience of a Spanish community hospital. Surg Endosc 2010;24:1701-1706.
28. Nagar AB. ERCP in the community: the benchmarks have been set. Gastrointest Endosc 2009;70:468-470.
29. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc 1998;48:1-10.
30. Cotton PB. Are low-volume ERCPists a problem in the United States? A plea to examine and improve ERCP practice-NOW. Gastrointest Endosc 2011;74:161-166.
31. Principles of training in gastrointestinal endoscopy. From the ASGE. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc 1999;49:845-853.
32. Endoscopy JAGoG. Guidelines for the training, appraisal and assessment of trainees in gastrointestinal endoscopy and for the assessment of units for registration and re-registration [Internet]; London: British Society of Gastroenterology; 2017. Jan. 11. Available from: https://docplayer.net/23468325-Guidelines-for-the-training-appraisal-andassessment-of-trainees-in-gastrointestinal-endoscopy.html.
Fig. 1.The number of diagnostic and therapeutic endoscopic retrograde cholangiopancreatographies performed in Korea. ERCP, endoscopic retrograde cholangiopancreatography. 
Fig. 2.The number of endoscopic retrograde cholangiopancreatography in various hospital types in Korea (2010 and 2014). 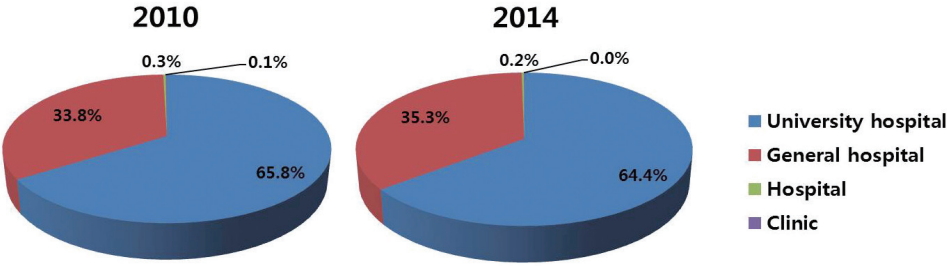
Fig. 3.Annual endoscopic retrograde cholangiopancreatography rates (per 100,000 habitants) in Korea and other countries. ERCP, endoscopic retrograde cholangiopancreatography. 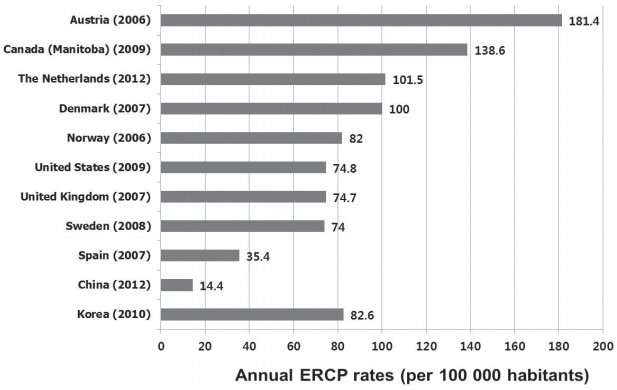
Table 1.Proportions of endoscopists who would perform ERCP for various indications stratified by degree of difficulty according to individual volume
Table 2.Proportions of endoscopists who would perform ERCP for various indications stratified by degree of difficulty according to hospital volume
Table 3.The frequency of actual use of the essential protective equipment and actual putting on radiation dosimeters |
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
|||||