INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is a well-known treatment of choice for removing common bile duct (CBD) stones. However, bile duct stones, especially those above the proximal CBD, are relatively difficult to remove through ampulla because selective deep bile duct cannulation into desired branched duct is often difficult or even impossible. Percutaneous transhepatic cholangioscopic removal with lithotriopsy of bile duct stone has been recommended if conventional endoscopic technique via ampulla fails. Unfortunately, the percutaneous procedure until the final session is time-consuming because tract maturation varies depending on the size of the final working sheath to remove stones. It usually takes more than 2–3 weeks for a 16–18 French working sheath. The rate of complications such as pain, cholangitis, bile leak, hemorrhage, and pneumothorax in percutaneous procedure for stone removal is 5–10% [1,2]. Endoscopic ultrasound (EUS)-guided procedure for bile duct disease has emerged as a more feasible and safer treatment than percutaneous transhepatic biliary drainage (PTBD) [3]. EUS-guided CBD stone removal and ERCP-guided procedure have been reported to have comparable outcomes in a previous report [4]. After creating a transmural tract through EUS-guided choledochoduodenostomy (CDS), the common hepatic duct and the proximal intrahepatic bile duct (IHD) can be explored with a slim and conventional gastroscope through the sinus tract in an attempt to remove difficult bile duct stones above the proximal CBD after ERCP-guided removal fails. A similar case of EUS-guided CDS with lumen-apposing metal stent has been previously reported [5]. We experienced three cases of successful removal of difficult bile duct stones above the proximal CBD via the tract created by EUS-guided CDS after failed ERCP.
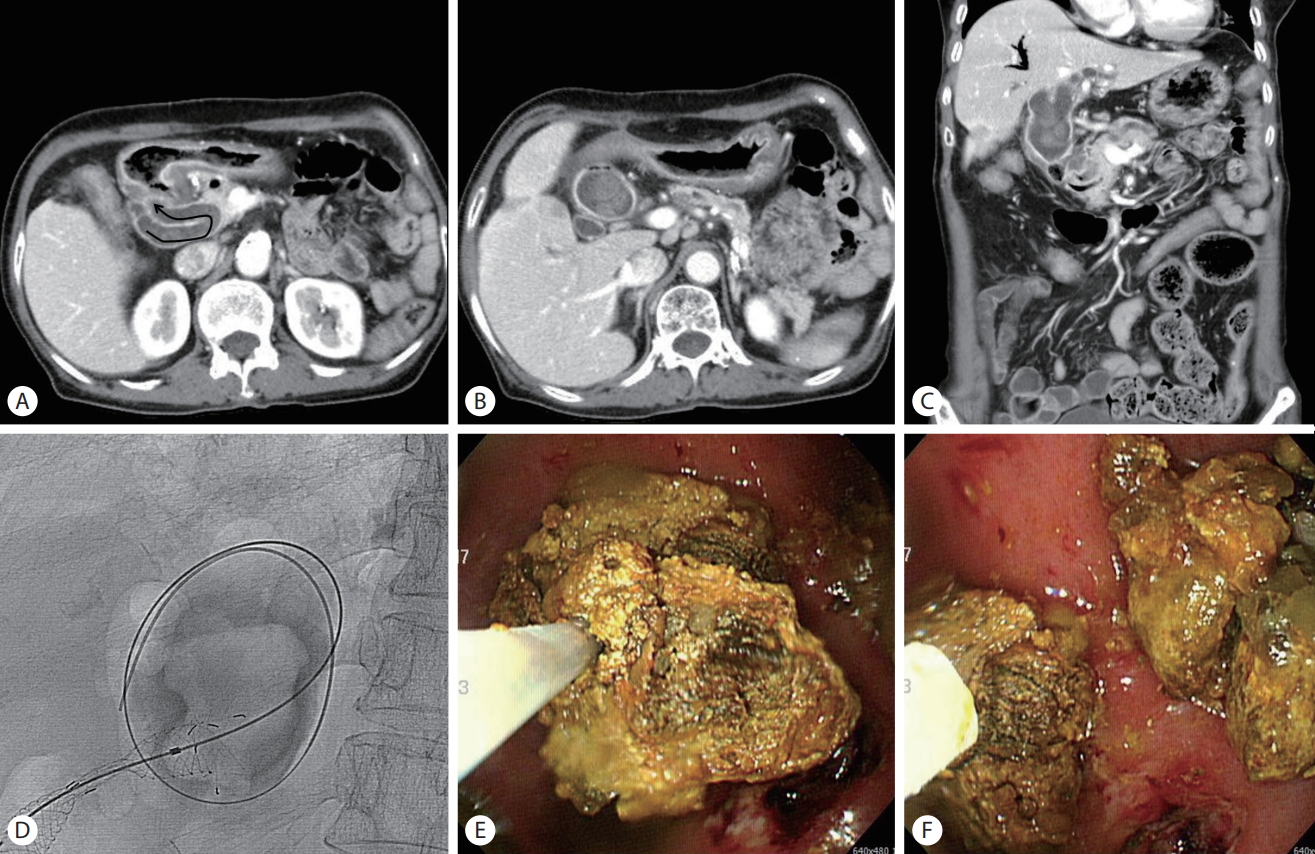
CASE 1
A 75-year-old female presented with abdominal pain and febrile sense. Her past medical history was pulmonary tuberculosis 25 years ago, spontaneous seroclearance of HBs Ag 10 years ago, diabetes mellitus under insulin therapy for 20 years, cerebral infarction 7 years ago under medication, and endoscopic removal of CBD stones one year ago. Her social history of alcohol and smoking was unremarkable. Her initial vital signs were: blood pressure, 110/70 mmHg; heart rate, 88 beats/min; respiratory rate, 20/min; and body temperature, 37.7℃. Physical examination showed tenderness of the upper abdomen. The remaining was otherwise unremarkable. Laboratory blood test revealed white blood cell count of 11,990/uL, aspartate aminotransferase/alanine aminotransferase of 381/160 IU/L, gamma-glutamyl transferase of 175 IU/L, total bilirubin of 1.1 mg/dL, and amylase/lipase of 62/33 IU/L C-reactive protein of 1.5 mg/L. Abdominal computed tomography showed severely dilated bile duct above the proximal CBD with multiple stones and acutely curved (black arrow) CBD (Fig. 1A-C). Initial approach by conventional ERCP for removal of stones nearly failed because deep insertion of the catheter into the bile duct was impossible due to deformed anatomy. We then performed EUS-guided insertion of covered biliary metal stent (BONA-AL stent, Standard Sci Tech, Seoul, Korea) from the duodenum into the proximal CBD. Five days after the procedure, these proximal CBD stones were successfully removed after removing the inserted metal stent using a conventional gastroscope with snare (Olympus, Tokyo, Japan), basket (trapezoid; Boston Scientific, Natick, MA, USA), and Roth-net retrieval (US Endoscopy, Mentor, OH, USA) (Fig. 1D-F). She has been doing well since then (14 months after the procedure).
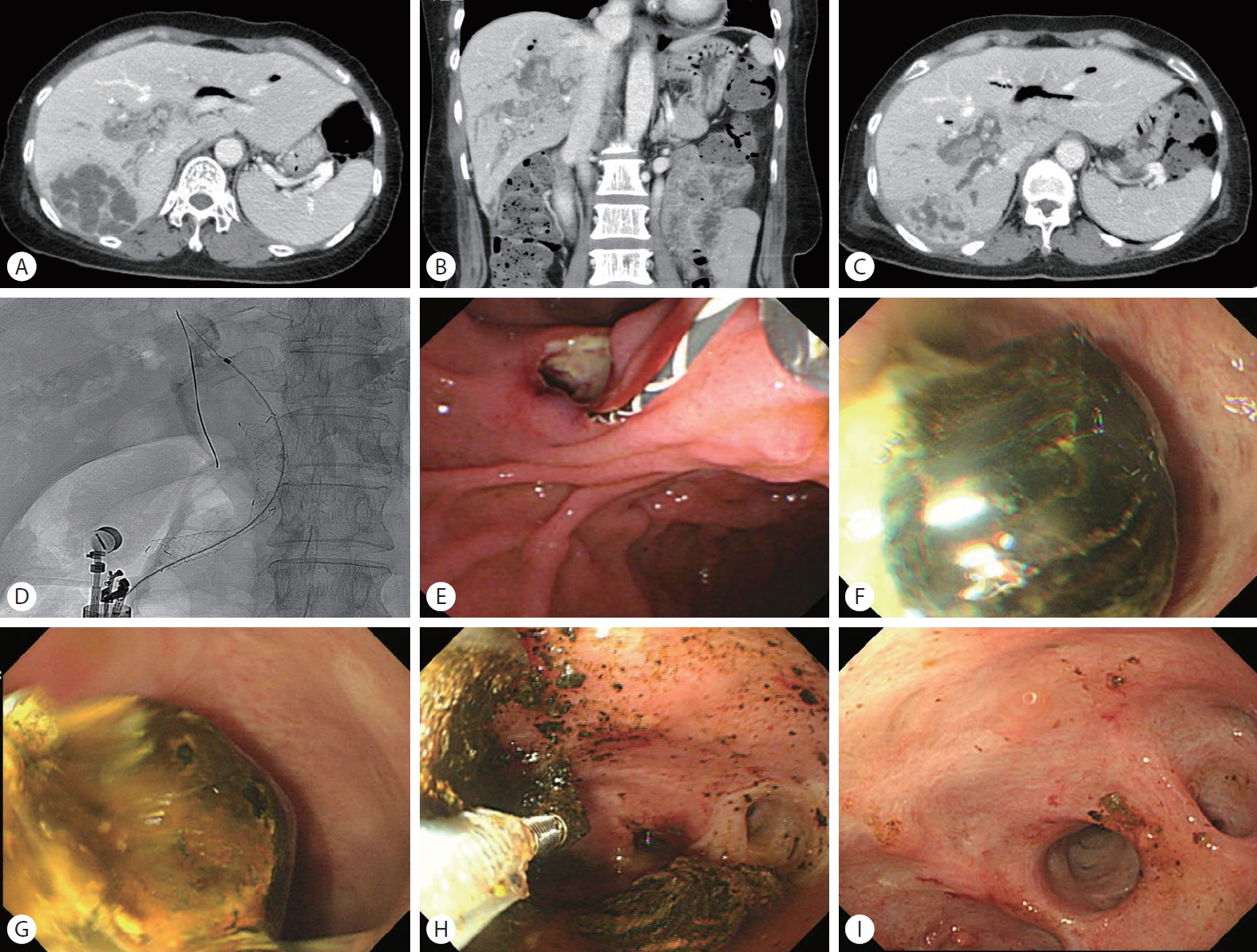
CASE 2
A 56-year-old female patient who presented with abdominal pain, vomiting, and fever that occurred 5 days ago visited SAM Hospital Emergency Center. Her past history included hospitalization and endoscopic removal due to bile duct stones in another hospital 10 years ago. Her vital signs were: blood pressure, 121/80 mmHg; heart rate, 80 beats/min; respiratory rate, 20/min; and body temperature, 38.9℃. She appeared acutely ill. Initial physical examination was tenderness in the right upper quadrant area. The remaining was otherwise unremarkable. Laboratory results were as follows: white blood cell count, 14,200/uL; hemoglobin, 12.3 g/dL; AST, 33 U/L; ALT, 41 U/L; albumin, 3.0 g/dL; ALP, 685 IU/L; C-reactive protein, 392 mg/L; alpha-fetoprotein, 1.4 ng/mL; and CA, 19-9 2.1 U/mL. Abdominal computed tomography showed approximately 80 × 65 mm hypoattenuating multiseptated round lesion with a well-defined margin in the right hepatic posterior lobe consistent of pyogenic liver abscess and multiple stones in right IHDs (Fig. 2A, 2B). The hepatic abscess was much improved after percutaneous catheter drainage and intravenous antibiotics for Escherichia coli from pus culture for two weeks (Fig. 2C). To treat further IHD stone-related liver abscess, we recommended surgical treatment of IHD stones. However, she declined. We then performed ERCP to remove those stones. However, it nearly failed. To easily access the IHD, we then performed EUS-guided CDS with a biliary covered metal stent (Standard Sci Tech) (Fig. 2D) and successfully removed IHD stones through the fistula tract using a conventional gastroscope with a basket (trapezoid; Boston Scientific) 5 days later (Fig. 2E-I). She has been doing well since then (11 months after the procedure).
CASE 3
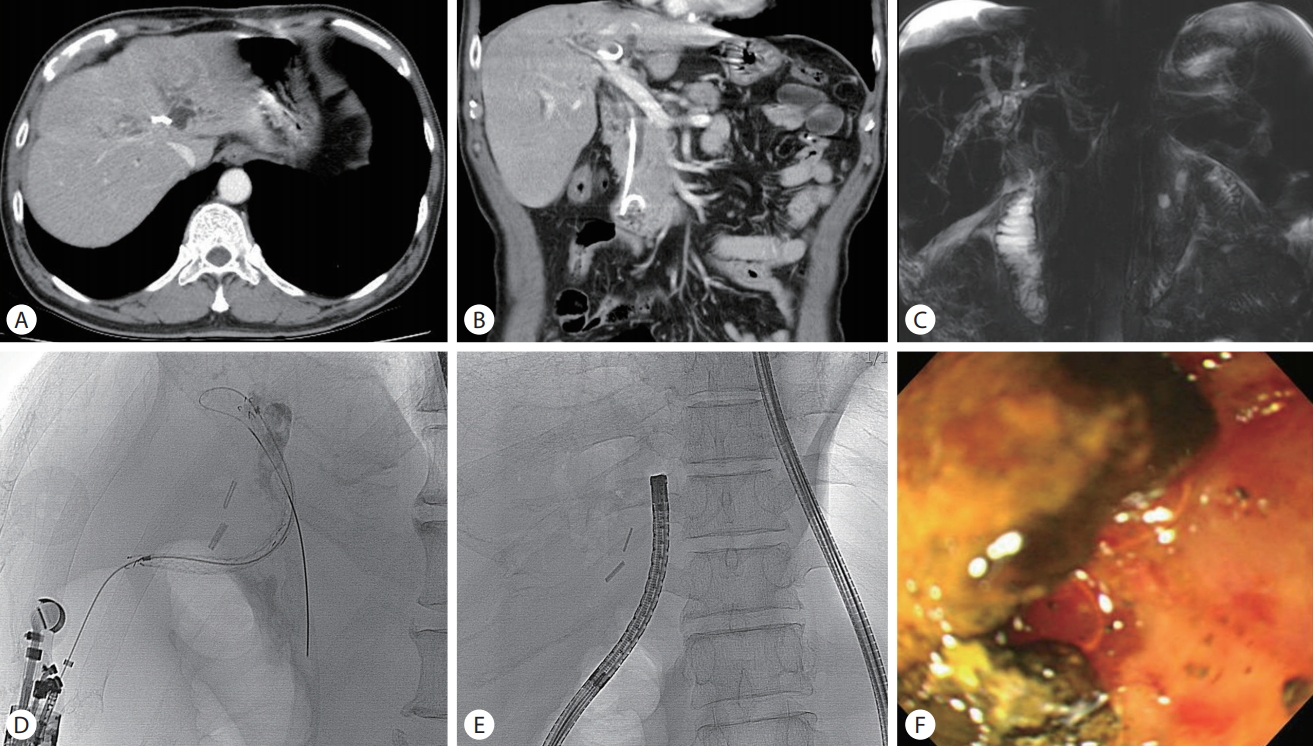
A 59-year-old male patient visited SAM Hospital due to yellow change of skin with severe itching and intermittent chilling sense 14 days ago. His medical history was alcoholic liver disease, cholecystectomy due to calculous cholecystitis two years ago, and endoscopic removal of bile duct stones due to cholangitis 3 months and 1 year ago. His social history was nearly daily intake of 80–160 g of alcohol and current smoker of one pack per day for 40 years. His initial vital signs and physical examination were unremarkable except for icteric sclerae with yellow skin on the whole body. Initial laboratory test showed AST of 51 IU/L, ALT of 45 IU/L, ALP of 922 IU/L, gamma-glutamyl transferase of 198 IU/L, total bilirubin 14.3 mg/dL (direct form: 10.4 mg/dL), CA 19-9 4.2 U/mL, HBs Ag negative, and anti-HCV Ab negative. Initial abdominal tomography and magnetic resonance imaging showed multiple tiny to small stones in the dilated left IHD and CBD with a well-placed biliary plastic stent in CBD (Fig. 3A-C). Initial removal of stones was performed by conventional ERCP. Although it was possible to remove CBD stones, the removal of IHD stones nearly failed. We then performed EUS-guided CDS with a biliary covered metal stent (Standard Sci Tech) (Fig. 3D). Five days after the procedure, most of multiple IHD stones were successfully removed after removing the inserted metal stent using a conventional gastroscope with basket (trapezoid; Boston Scientific) and Roth-net retrieval (US Endoscopy, Mentor, OH, USA) (Fig. 3E, 3F). His itchy sense with yellow skin gradually improved. He was discharged 5 days later after the last procedure. He has been doing well since then (9 months after the procedure).
DISCUSSION
IHD stone refers to the presence of calculi located proximal to the confluence of left and/or right hepatic ducts. IHD stone is classified according to its origin. Primary IHD stone is prevalent in East Asia. It is commonly accompanied by biliary stricture. Secondary IHD stone is formed from CBD stone and GB stone. The age of predilection is between 40 and 50 years of age. The incidence of IHD stone varies. It is relatively common in Asia, with a rate ranging from 2 to 25%. Its incidence is rare in Western countries, with a rate of 0.6 to 1.3% [6].
The etiology of IHD stone is not well understood yet. Malnutrition and low socioeconomic status have been suggested to contribute to the development of IHD stones. Westernized diet in Asia has changed the pattern of gallstone disease, showing an increase in the prevalence of gallstone but a decrease in the prevalence of IHD stone [6,7]. Parasitic infection is another major cause for the formation of IHD stone. Parasite has been detected in up to 30% of IHD stones [6]. Clonorchiasis is especially endemic in East Asia, although parasite infection has decreased nowadays. Additionally, cholestasis can affect bile production and excretion. Anatomic abnormality of bile duct such as choledochal cyst, Caroli’s disease, and imbalance of bile components related to bile metabolic defects may also cause IHD stones [8].
The natural history of IHD stone is not well elucidated yet. Clinical manifestations of IHD stone include repeated events of abdominal pain, fever, and jaundice with bile duct dilatation in image studies. Symptomatic IHD stone must be treated to prevent liver abscess, biliary cirrhosis, portal hypertension, hepatic failure, and cholangiocarcinoma. IHD stone is an established risk factor of cholangiocarcinoma. Cholangiocarcinoma can occur in 2–13% of patients with IHD stone [6,9].
Treatment goal of IHD stone is to completely remove the stone. However, IHD stone removal is complex. Moreover, disease progression occurs in most patients even after adequate treatment [10]. Surgery is strongly considered for relatively young patients with liver abscess and suggested biliary stricture like case 2. Surgical treatment is traditionally the standard of treatment. However, recurrence occurs frequently although various techniques have been used for surgical treatment [9]. In fact, surgery is sometimes very difficult and even impossible in patients with complex IHD stones and poor general conditions who are mostly older in age with comorbidities such as cardiovascular disease, pulmonary disease, and/or diabetes mellitus. According to previous studies, the incidence of postoperative complications is 12.0–38.5% after liver resection, 24.3–38.0% after hepaticoenterostomy, and 2.1–40.0% after intrahepatic duct exploration [9]. Therefore, treatment for IHD stones requires multidisciplinary approach, including minimally invasive surgery in combination with endoscopic and radiological treatment before and after surgery. The principal approach to IHD stone is surgical exploration of bile duct with stone removal by biliary drainage or hepaticojejunostomy (with or without access loop construction), hepatic resection, and percutaneous transhepatic cholangioscopic lithotripsy. Success rates of the above treatments range from 72% to 92% [10]. Percutaneous transhepatic cholangioscopic lithotomy or lithotriopsy is nowadays commonly used for the removal of IHD stone or difficult cases of CBD stone [11]. Transpapillary endoscopic treatment with ultraslim endoscopy can be another option to access the IHD to remove the stone [12,13]. However, this procedure is technically difficult sometimes.
PTBD is also a well-established primary or palliative procedure for pancreaticobiliary disease causing obstructive jaundice such as stone or tumor with relative safety and efficacy. This procedure is often regarded as a rescue therapy for failed ERCP attempted for difficult CBD stone or IHD stone which occurs in approximately 6–7% of cases with altered or variant anatomy such as periampullary diverticulum, gastric outlet obstruction, and gastric bypass surgery [14]. Percutaneous removal of bile duct stone with occlusion balloon with or without basket is a safe and effective alternative approach in selected patients [15,16]. PTBD-based removal of difficult CBD and multiple IHD stones is a relatively time-consuming and complicated procedure which sometimes needs repeated tract dilatation for insertion of choledochoscopy with a diameter of approximately 5 mm. Insertion site pain of the drainage catheter frequently occurs during and after multiple procedures. Other complications like fistula formation and recurrent injection need a long-term external drainage catheter that leads to a poor quality of life [11]. With advance of therapeutic EUS techniques and equipment, EUS-guided drainage procedure has been used in pancreaticobiliary diseases such as stone or tumor causing obstruction of biliary and pancreatic duct or gallbladder [14]. Based on the idea that easy insertion of conventional gastroscope with diameter of 9–10 mm or ultraslim endoscope of diameter of 5–6 mm through the sinus tract made by EUS-guided CDS can comfortably access the IHD, EUS-guided procedure instead of the conventional PTBD-based procedure might be useful. In addition, EUS-guided procedure can be performed in the same endoscopy room in one session after failed ERCP. We actually performed the removal of proximal CBD and IHD stones 5 days after EUS-guided insertion of CDS stent due to the development of self-limited bleeding and the possibility of stent migration caused by immature expansion of stent during consecutive manipulation of accessory for the removal of stones. The required time from admission to the day of discharge after removal of difficult bile duct stones was 10–14 days. It was generally shorter than the required time related to PTBD-based removal of difficult bile duct stones in our experience. However, the sinus tract after removal of CDS metal stent can later predispose ascending cholangitis in these patients, which is an unresolved problem or limitation. Long-term follow-up is needed for detecting late complications of ascending cholangitis in these patients after the removal of bile duct stones by CDS in comparison with other procedure including conventional ERCP. Fortunately, all three patients have been living well (for more than 9 months) based on the last follow-up.
This ongoing interim study showed that removal of difficult bile duct stone through the sinus tract by EUS-guided CDS could be an effective, safe, and simple alternative for patients with failed ERCP compared to PTBD-based procedure.